| Q&A with John A. Hartford Foundation President Rani E. Snyder
| On January 1, Rani E. Snyder, MPA, became president of The John A. Hartford Foundation, a leading private foundation dedicated to improving care for older adults. Previously vice president of program, Snyder reflects here on her approach to partnership, advocacy, and building an age-friendly ecosystem.
Now that you’re president of the foundation, what’s on the horizon, in terms of strategy?
I’m excited and energized to continue advancing our mission and priorities, which are not going to change. We’ll remain solid and steadfast partners with our grantees because together, we’ve generated incredible momentum to spread age-friendly care that supports older adults and their family caregivers. We’re not pulling back in any way, and at the same time we’ll move in some new directions with new partners that can advance our work, especially given the current policy environment.

What are some examples?
In the past year, we funded KFF to do a prospective analysis of potential changes in the policy realm, before they come down the pike, so that they could put information out to inform decisions. So that’s in areas like Medicaid, where we highlighted the often untold story of what cuts would mean for older adults, whether they are receiving nursing home care or home- and community-based services. This also included promoting congressional action on the Older Americans Act, one of the most important but unrecognized federal policies that effectively and efficiently serves 1 in 6 older adults in every community across the country.
Can you say more about that?
The Older Americans Act is low-hanging fruit. It’s really important and there’s bipartisan support. It makes sense economically, with a return on investment for states of about $2 for every dollar invested in essential local services like meal delivery, transportation to medical appointments and caregiver support. That may not sound new and sexy, but when we tell the story to policymakers about the real-world impact on the lives of older adults and how it prevents costlier hospitalizations and nursing home admissions, that gets attention. We thought it was going to be passed before the year ended, but the last government shutdown got in the way. We still think there’s a good chance for reauthorization in the coming year.
How do you prefer to work with grantee organizations?
We are somewhat unusual as a funder, in that we don’t just make a grant and walk away. Our staff work shoulder to shoulder with our grantees to ensure that the initiatives we fund have the biggest chance of success and greatest impact possible. Our program officers are experts. They help grantees problem-solve, course-correct and find additional resources.
Can you elaborate?
For example, we are constantly working to make connections to other funders to augment our grant funding. It also means “cross-tabbing” the grants that we fund in one of our program areas to grants in other areas, so that we’re all integrating to the greatest extent possible and rowing in the same direction. A great example is how we’ve connected several of our programs that support family caregivers with quality improvement initiatives working to make health care more age-friendly. Coordination is amplification, and that’s what we’re looking for.

What is your approach to partnerships?
As I described, our grantees are always very important constituents and partners. Other partners help get us to the impact we seek, and they absolutely include other funders. We do a very good job of partnering with other foundations. We are a national private philanthropy devoted solely to aging and health. Other funders in aging operate differently and may focus on economic security or other aging topics. Many of these foundations also operate within a given state, community or geographic region, whereas we fund nationally. Increasingly, we have recognized that the action is moving more and more to states, and so partnership with state and local funders has become even more important. Understanding our fellow funders and how they work is key. Because we’re a national funder, we also partner closely with federal agencies to move regulatory policy whenever possible, which is unusual for foundations.
What social trends are you following?
We have been following the trend of looking at social isolation and loneliness, although we frame it as ‘social connection,’ and exploring the ways that we can both understand that issue specific to older people and build that into age-friendly care. We have a grant that is under way right now with USAging, which is the national organization for all of the nonprofit aging services organizations in communities across the country, including Area Agencies on Aging.
How does this work build upon the foundation’s legacy?
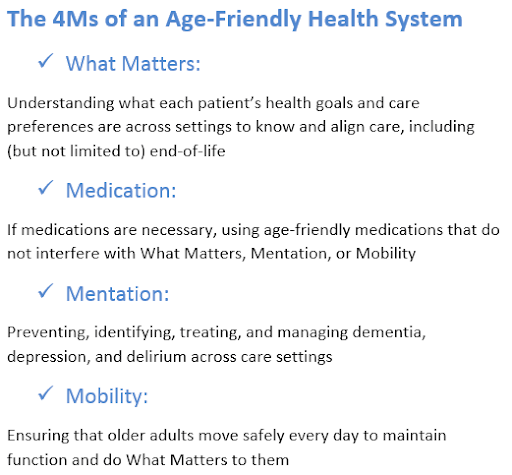
We are very proud to have helped build the field of geriatrics and, to a lesser degree, gerontology. We had a major focus on developing a stronger health care workforce that could care for an aging America. We first began in medicine with our centers of excellence in geriatrics across the country, then added nursing and social work with similar academic centers of excellence and fellowships to support leaders in research, education and practice. One of the things that we realized is that we needed a different kind of approach to spread and scale good geriatrics care than going university by university. At the same time, we built not only expertise in geriatrics and gerontology but also funded the development of some really amazing models of care. The problem was they weren’t reaching all of the people who could benefit from them. So that’s part of the reason that we shifted to thinking more about those national organizations that can change health care systems, rather than focusing only on academic institutions. We’re now building age-friendly health systems in partnership with organizations like the Institute for Healthcare Improvement, with whom we developed the 4Ms framework, and the American Hospital Association, which has been a leader in this work as well. It’s really about systems change and implementing the framework to change behaviors and clinical practice, regardless of whether someone is a geriatrician or a gerontological nurse or nurse practitioner.
What technology trends do you think will affect the field?
We are looking at AI and other tech solutions. In fact, sitting on my desk, the next thing I’ll do after we get off this call, is a new grant proposal from UTHealth to test the ways that we can use AI to help care planning based on asking what matters to older adults. We’re looking for the ways that AI can not only simplify the asking, but more importantly the recording and the acting on what matters so that the treatment and care plan are aligned with an older patient’s goals, values, and preferences.
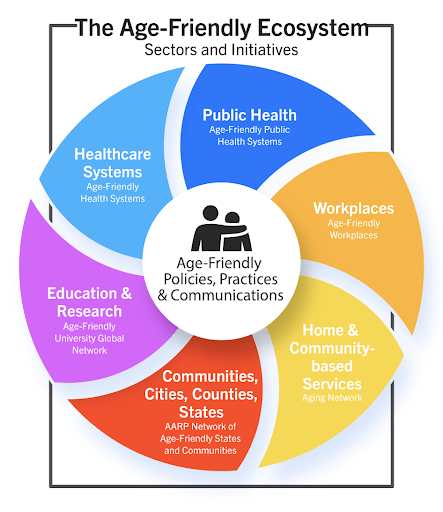
How does that tie in with the idea of an age-friendly ecosystem?
In addition to our age-friendly health systems work, we support Trust for America’s Health, which is a national public health nonprofit. They’ve been helping us think through what it means to have an age-friendly ecosystem, which means that all sectors of society are adapting to the needs of an aging population. There’s a whole global network, and it includes things like age-friendly health systems as well as age-friendly public health systems, age-friendly communities and even age-friendly universities. It is a whole-of-society approach. The World Health Organization and AARP are our partners in developing and promoting these strategies.
How did you first get involved with this work?
Oftentimes when you speak to people in the field of aging, they’ll say, ‘Oh, it was a relationship with my grandmother or grandfather,’ or someone who was older who was really meaningful to them. I think my interest was more intellectual. I love that my very first job out of college was actually at The John A. Hartford Foundation more than three decades ago, before going to other philanthropies focused on aging like the Commonwealth Fund and Donald W. Reynolds Foundation. At first, I didn’t yet know what philanthropy was. And our foundation had another program area. But now, our mission is solely to improve the care of older adults, and that’s what we eat, sleep, and breathe, professionally speaking. I recognized that demographics were changing in challenging ways and that we were going to need a lot of time and dedicated attention to meet the needs of an aging population. We’re still working on that, all these years later.
What would you tell yourself back then about what lay ahead?
I would say that there’s nothing more important than building partnerships. It comes down to cultivating and creating strong relationships, which includes understanding who your current or potential partners are, making sure that you are respecting the different ways that they—either by culture or organization—can and do interact and accomplish their work. And then it’s about building that understanding and consideration into the way that we all work together. That’s what’s important for getting things done.

Leave a comment