| Turning Momentum into Action
| Bob Blancato and Laura Borth
| Malnutrition threatens the health and independence of as many as 50% of older adults and causes tens of thousands of deaths each year. The crisis incurs more than $51.3 billion in health costs annually.
When Senator Chris Murphy and Representative Suzanne Bonamici recognized Malnutrition Awareness Week, which just passed, they highlighted the importance of federal nutrition programs and community-based organizations in preventing malnutrition and its devastating effects.
As proud leaders of the Defeat Malnutrition Today coalition, we are deeply committed to this vital cause and join the American Society for Parenteral and Enteral Nutrition (ASPEN) to raise awareness year round. But awareness alone is not enough; lasting change requires stronger policies and better data to guide prevention and treatment.

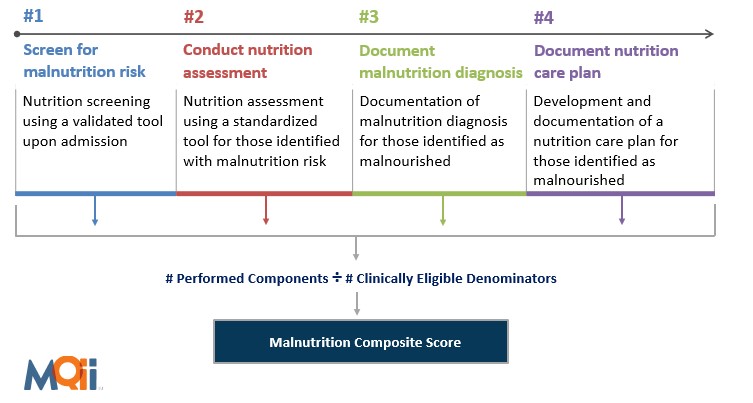
One of the most important steps forward is the Malnutrition Care Score (MCS), a Centers for Medicare & Medicaid Services (CMS) quality measure that evaluates how well hospitals screen for malnutrition risk, diagnose it, and develop a care plan. CMS first adopted MCS as a voluntary reporting measure for patients 65 and older and in 2024 expanded eligibility to all adults. The next logical step is mandatory reporting so every patient can be identified early and connected to help. Momentum from Malnutrition Awareness Week can drive that change, ensuring hospital screening translates into real community support. Awareness and hospital reporting only matter if there is somewhere to refer people once they are diagnosed.
Defeat Malnutrition Today, a broad alliance of 130 organizations is turning awareness into action, addressing these issues through federal policy, especially looking to bridge the gap between healthcare settings and the community programs older adults rely on every day.
Congress recognized this urgency in the 2020 reauthorization of the Older Americans Act (OAA), when lawmakers added reducing malnutrition to the very purpose of the Act. They also updated the OAA’s disease prevention and health promotion services to include screening for and addressing malnutrition. Community programs funded under OAA provide home and community-based services, including home-delivered and congregate meals and nutrition education, and are ready-made referral partners when hospitals identify malnutrition risk. According to the National Survey of Older Americans Act Programs (NSOAAP), 1 in 5 were at risk for malnutrition, while older adults receiving home-delivered meals for 2 to 5 years were 72% less likely to be at risk than those served for 6 months or less.
As we look ahead, there is a bipartisan opportunity to further advance policies to help prevent malnutrition from Malnutrition Care Score reporting from hospitals, a possible OAA reauthorization, to inclusion of the Medical Nutrition Therapy Act and Treat and Reduce Obesity Act in an end-of-year legislative package. The momentum from Malnutrition Awareness Week will help especially in ensuring that CMS’s Make America Healthy Again effort addresses proper nutrition at every age—not just in childhood. Everyone is aging, and prevention should follow us from pediatric visits to later years.
Malnutrition Awareness Week is more than a date on the calendar—it is an invitation to screen and refer older adults to appropriate community nutrition programs and nutrition counseling. We must also strive to make foods that keep older adults and others healthy accessible and affordable. Good nutrition is as powerful a preventive measure as we have; we just need to recognize and support it. If we are what we eat, then let’s make sure it is nutritious.
Robert Blancato is National Coordinator and Laura Borth is Policy Director of the Defeat Malnutrition Today coalition.

Leave a comment