Eric Goldwein
I spend a lot of time digging through spreadsheets. Since 2019, I’ve been analyzing staffing levels in U.S. nursing homes using the Centers for Medicare and Medicaid Services’ Payroll-Based Journal (PBJ) data — a trove of audited records that track every nurse and aide hour worked, in all 15,000 facilities, every day since 2017. The findings are clear:
- Most nursing homes are understaffed — 9 out of 10, based on new methodology that accounts for resident acuity. Most aren’t even close.
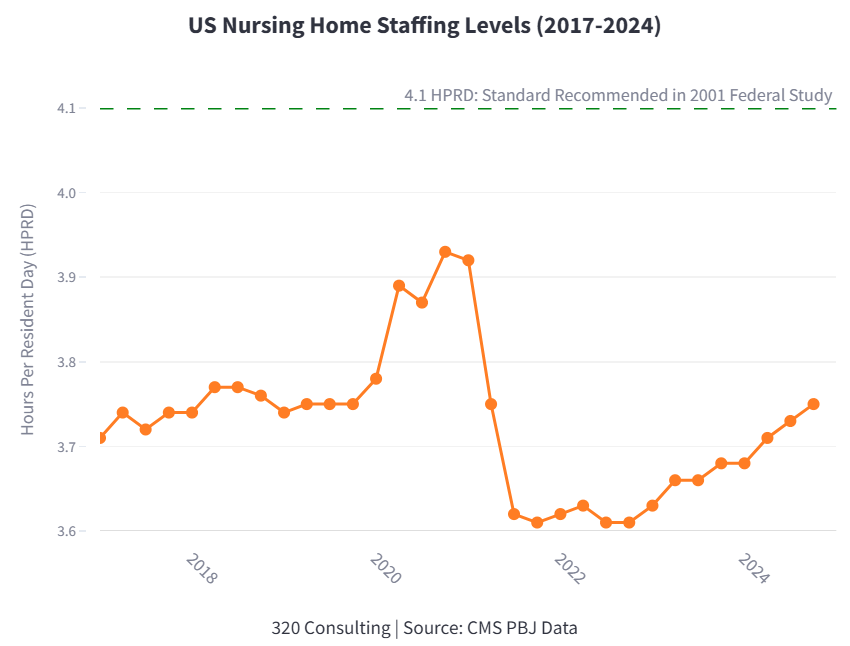
- The typical nursing home provides 3.69 total staff hours per resident per day (HPRD), far below the 4.10 recommended by a federal study. Night, weekend, and holiday staffing is much lower.
- Turnover is high. Nursing homes lose nearly half their staff each year, and churn is even higher when measured by hours.
But here’s the thing: you don’t need a spreadsheet or a regression model to know nursing homes are understaffed. Just walk into your uncle’s five-star nursing home, smell the urine, and watch one nurse aide try to do the work of two.
Or ask a resident. They’ll tell you the staff work hard but are stretched thin. Sometimes there’s not enough to wheel them outside or fix the TV before a Yankees game.
Michael Wasserman, a geriatrician and former CEO of a nursing home chain, has been raising these concerns for years. “Whether it’s changing diapers or answering call lights or taking someone to the bathroom — if you have one person and 20 residents, it just ain’t gonna happen,” he says.
Research consistently links lower staffing with worse outcomes — pressure ulcers, falls, hospitalizations, COVID, you name it. And yet most nursing homes operate well below the recommended levels and are rarely held accountable.
Unfortunately, a federal staffing standard isn’t going to save the day. In April, the courts struck down a mandate requiring 24/7 RN coverage and a modest but meaningful minimum staffing standard.
As it stands, nursing homes are required to “provide enough nursing staff every day to meet the needs of every resident” — a standard as enforced as it is quantified. In 2024, the F725 staffing citation was handed out a total of 979 times. Only 30 of those citations (one for every 500 nursing homes) amounted to more than a slap on the wrist.
“That’s the great danger of the minimum staffing standard going away,” Wasserman says. “There will be no accountability for the worst actors who dramatically understaff the facilities.”
Some states have minimum staffing standards. While not a cure-all – they are often underenforced or easily gamed – perhaps they can help. States like Oregon and North Dakota, which have such standards, consistently rank near the top in staffing levels.
Still, more must be done. With an aging population, more Americans will end up in nursing homes unequipped to care for them. PBJ data helps us see the patterns — and spotlight the facilities and regions most in need. But with the federal path blocked, progress will depend on states, on advocates, and on anyone still willing to fight for the dignity and safety of nursing home residents.
Eric Goldwein helps small teams and nonprofits turn messy data—like PBJ spreadsheets—into user-friendly tools and compelling stories. Learn more at 320 Consulting.
Leave a comment